Contents menu
1. Introduction
The Health Data Research UK (HDR UK) Patient and Public Involvement and Engagement (PPIE) team commissioned this review to collate existing literature on public attitudes towards the collection and use of their health data across the UK. In some cases, where evidence is unavailable, attitudes to health research, more broadly, are used as a proxy.
For our PPIE work at HDR UK, this document provides clarity on what we might mean by ‘underserved’ audiences in public engagement with research that uses health data (health data research). It is shaping our next steps in developing approaches to work with audiences who are not engaged as part of our 2024 – 2028 PPIE Strategy. The review also highlights key gaps in public attitude research towards health data, gaps we hope the sector will collectively work to address.
We hope this document proves to be useful beyond HDR UK and that it will support the wider data research community in identifying and reaching new audiences in your own public engagement activities.
If you’ve found this document helpful, have any questions, or you’ve got relevant research you would like to share please get in touch at involvement@hdruk.ac.uk.
2. Background
2.1. Attitudes towards health research
Public attitudes towards health research in general are positive. A 2023 Health Research Authority (HRA) survey[1] shows that two-thirds are confident it improves people’s lives, and 68% say they would be willing to participate in research if asked.
However, this does not tally with the numbers actually participating in health research. A 2021 National Institute for Health and Care Research (NIHR)[2] report demonstrates the disconnect between the opportunities to be involved in health research and people’s awareness of them. Despite every single UK hospital offering opportunities to be involved in research, only 13% of the public were aware of this.
2.2. Attitudes towards health data
Surveys also highlight that although people may be supportive of health research for both individual and societal benefits, they are not familiar with the concept of health data research or the ways to be involved. A 2023 Health Foundation report[3] for example, found that over 60% of respondents knew very little or nothing at all about how the NHS is using the health data it collects.
More specific research into public attitudes towards sharing health data – both identifiable and de-identified – demonstrates consistent trends (see Figure 1 for different types of data identifiability). People are willing to share data when they know who is using it and why. The 2023 Sudlow review[4] of the UK health data landscape highlights that people in general support the use of their health data for both their own and a wider societal benefit, but they want to know how and why it is being used. This reflects themes common to many public dialogues about new technologies and areas of scientific research – people value transparency and societal benefit, being more open to research when it benefits the whole of society (as opposed to business) and has clear regulation[5].
Local NHS services have the highest percentage of people trusting how they handle patient data (72%) in a 2024 public attitudes survey[6], with universities and charities coming next (56% and 58% respectively). This drops drastically for pharmaceutical companies (40%) and central government (46%) with commercial tech companies having the least trust (27%). The public are also particularly wary of sharing data that may be used for marketing or insurance purposes[7].
This hasn’t always been the case. A Wellcome-commissioned Ipsos report in 2016[8] showed that over half (54%)
of the public were willing to share health data with commercial organisations undertaking health research and 37% supported companies marketing health products.
However, since 2016 there have been numerous high-profile cases highlighting the risks of data sharing and the public demand for opt-in rather than opt-out data sharing. These include the collapse of the care.data project[9], scandals such as DeepMind acquiring 1.6 million patient records from the Royal Free London NHS Trust Foundation[10] and the campaign against the rollout of the General Practice Data for Planning and Research (GPDPR) scheme[11].
More recent studies such as the NHS 2024 survey[6] indicate that 40% would be willing to share data with pharmaceutical and medical research companies, a decrease from Wellcome’s 2016 findings.
It is important also to consider other external factors in public attitudes and awareness of health data. During the COVID-19 pandemic, data played a critical role in tracking disease and identifying communities most at risk[12,13]. With the government regularly publishing data and the media reporting on it, the pandemic has likely had a significant impact on how the public feel about sharing health data. A 2021 survey[14] found support for data sharing increased during COVID-19, but only for those organisations already trusted.
The rise in the use of Artificial Intelligence (AI) in healthcare is also likely to affect public opinion. In January 2025, the Labour government announced a new AI strategy with the possibility of sharing health data with the NHS and commercial companies[15], the impact of which has yet to be seen.
2.3. The digital divide
Public attitudes towards sharing health data cannot be discussed without also considering the importance and relevance of the digital divide[16]. Data and how it is shared is primarily electronic, and so for those groups who have limited or no access to the internet, or who are not confident with its use, there are additional challenges.
There is limited research into the impact of digital exclusion on attitudes towards data sharing, health or otherwise. Most reports referenced here used online methodologies such as web surveys, which will naturally bias towards those with digital access. Further discussion on digital access and attitudes towards health data sharing can be found in section 3.5.
2.4. Types of data shared
While in general people are comfortable with sharing their health data if certain conditions are met, there are further nuances with regards to what types of data people are willing to share.
In general, there is less support for sharing data on mental health or sexual information. This is evidenced strongly in a research paper on attitudes of people living with long-term health conditions[17], with participants most willing to share sleep data and least willing to share sexual orientation, health and activity.
Some reports have also looked at the impact anonymisation makes on attitudes towards data sharing. The Health Foundation report[3] found slightly less support for sharing identifiable health data compared to anonymous data, but still relatively strong support for it in certain scenarios; 70% were happy to share anonymous data with the NHS to understand disease risk, which dropped only slightly to 64% for identifiable data. When it came to sharing data with universities there was a bigger difference, with 65% supporting anonymous data sharing and 51% identifiable health data sharing.
Again, this reflects the broader trends of trust in organisations outlined in section 2.2 of this report, and how trusted they are to look after people’s data.
There has been limited research done on public attitudes towards sharing health data from personal devices such as fitness watches. A recent project from the British Heart Foundation Data Science Centre[18], hosted by HDR UK, showed that 75% of people were happy with the idea of linking their smartapp data to their NHS data. Acceptance was higher for passive data such as heart rate rather than active data such as self-reported mood.
2.5. Consent models
There are many types of consent models for collecting data, with the primary one used by the NHS being an opt-out model.
Very few surveys into attitudes towards sharing health data have gone into depth on the use of different consent models, but those that have suggest that who the data is being shared with is of more importance than the consent model used to share it. Whether this is due to lack of understanding of different consent models, or trust in organisations, is not clear.
A 2019 research paper[19] looking at attitudes towards reuse of health data among people in the EU found a muddled picture, with people in general supporting the re-use of health data as long as it provides societal benefit, regardless of the consent model. This is particularly true when the data is anonymous, although a 2013 survey in Ireland[20] found people wanted consent to be sought for every use of the data, whether anonymous or identifiable. However, the landscape around data use, consent and public awareness has changed in the decade since and this may no longer be reflective of current attitudes.
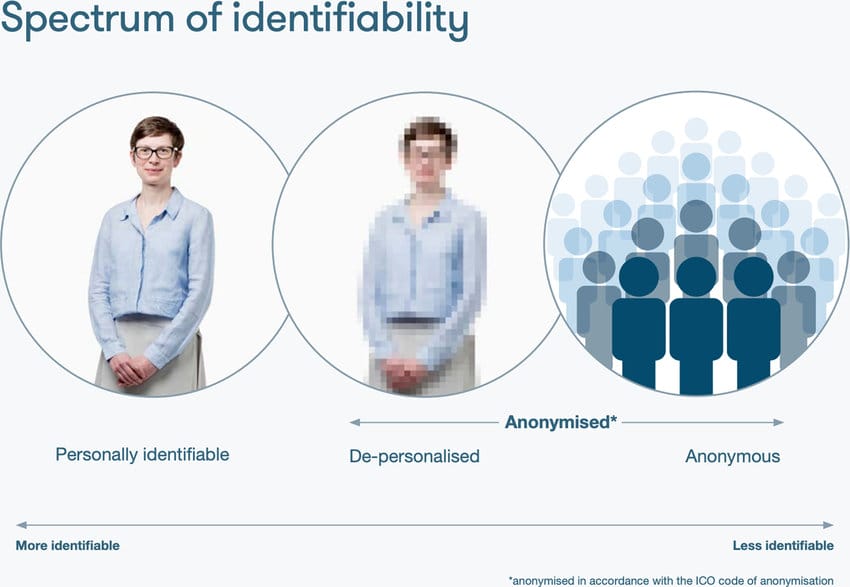
Figure 1. Visualisation of concepts of identifiable and anonymous data from Understanding Patient Data[21]. Personally identifiable information identifies a specific person; de-personalised data is about an individual but does not identify them, however it could be possible to re-identify the individual. Anonymous data is information from many people combined together, with individuals not identifiable.
3. Breakdown of trends
A detailed breakdown of demographic trends will help identify target audiences for HDR UK’s public engagement work. However, much of the literature on public attitudes towards health data is limited in demographic analyses.
One of the most comprehensive reports, undertaken as part of the NHS England’s digital transformation
project – data saves lives – is the survey of English public attitudes towards data in health and social care in 2024[6]. The headline findings were that 83% of people trusted the NHS to keep their patient data secure and that data security and cyber-attacks were people’s biggest concerns. The report segmented people into six groups. Although this was an England-only survey, attitudes in devolved nations have followed similar trends. Section 3.3 below provides further information on the impact of geographic locations.
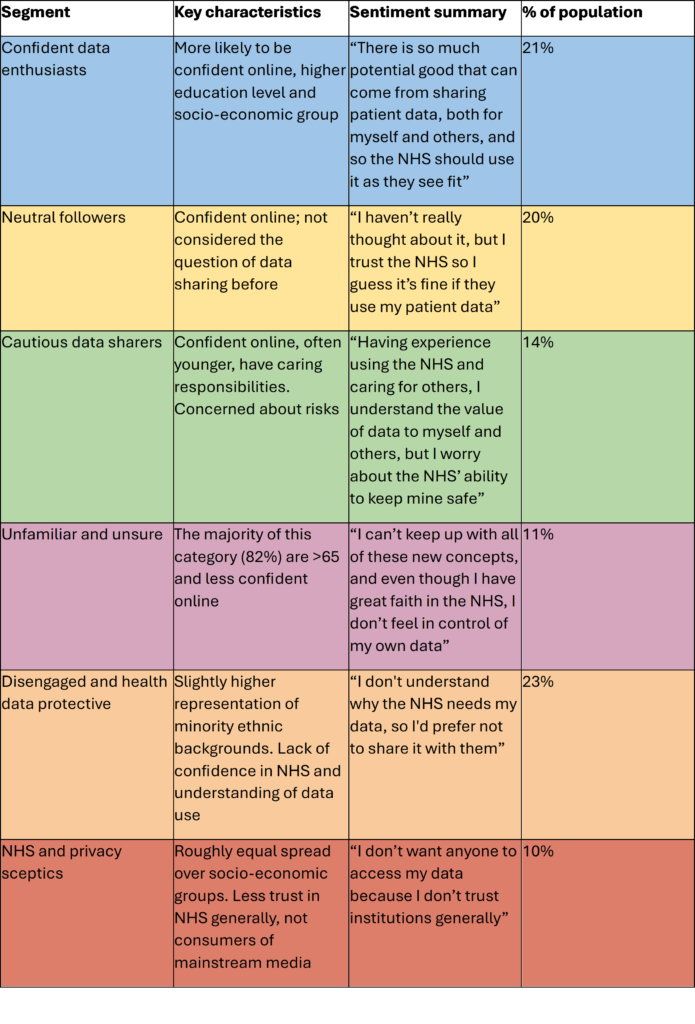
Table 1. Segmentation of English public into six groups according to attitudes towards sharing health data[22].
The HRA’s 2023 report[1] on public attitudes towards health research also provides some in-depth breakdown on attitudes by demographics (Figure 2).
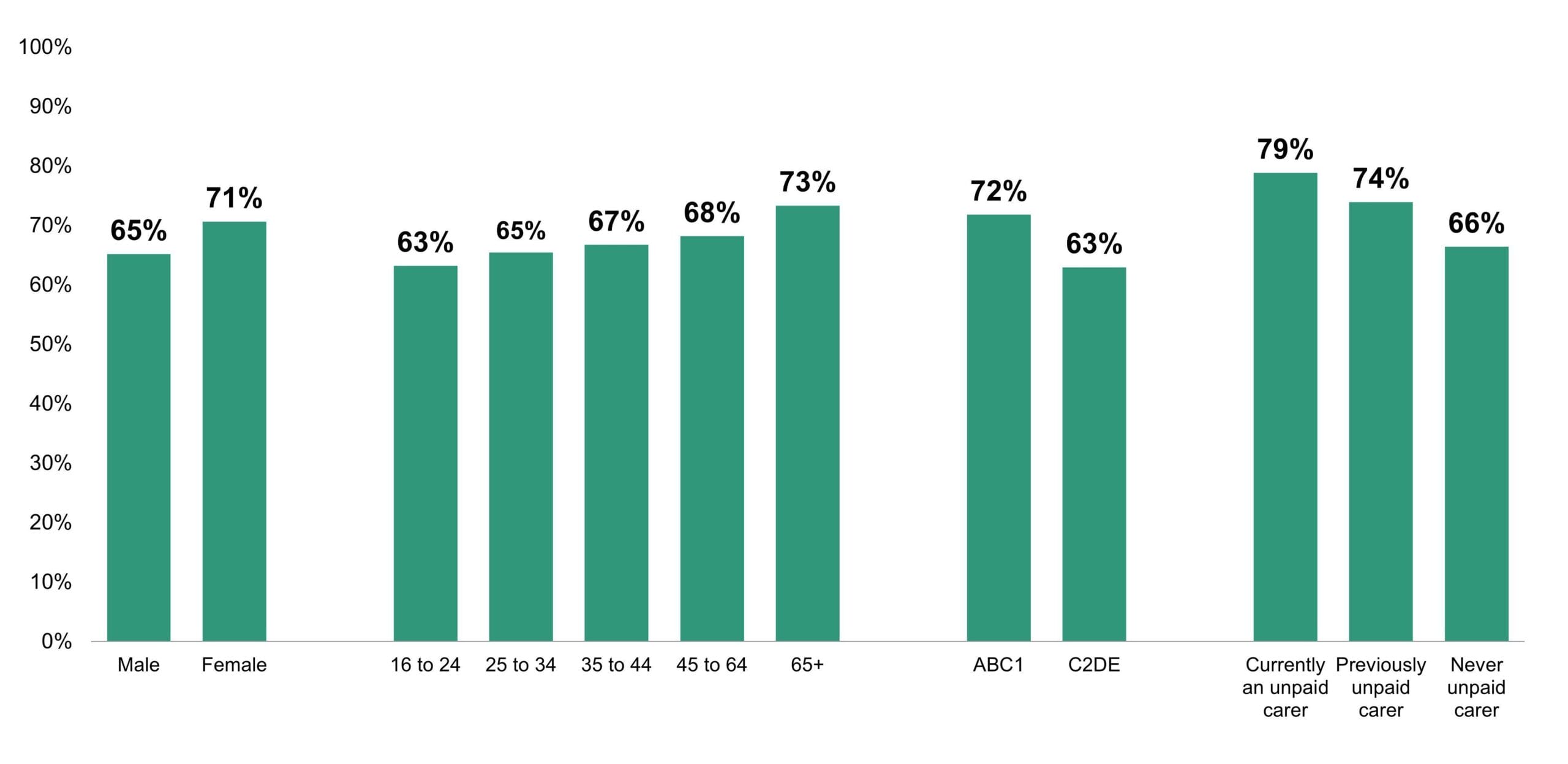
Fig 2: Results by demographic from HRA 2023 survey[1] of 5030 participants when asked: Imagine you were asked to take part in a health and social care research study. How likely would you be to take part? ABC1 are the three higher social and economic groups based on occupations, C2DE are the lower groups. These definitions are from the Market Research Society[23].
3.1 Gender
There is limited data on how gender impacts attitudes towards health data sharing. The closest proxies are attitudes towards health research and healthcare technology, with the HRA survey[1] showing women are marginally more likely than men to take part in health research (71% versus 65%, see Figure 2). The Health Foundation report[3] showed that men were consistently more positive about the benefits of health technology than women (Figure 3).
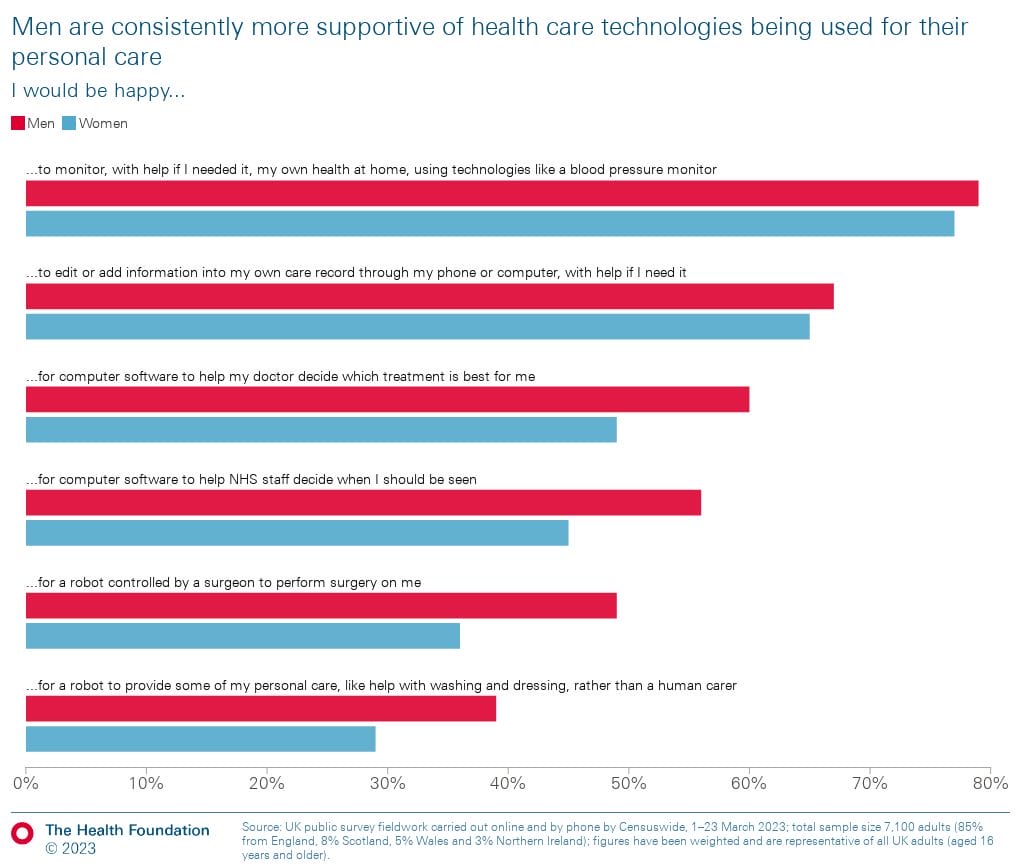
Fig 3: Attitude towards healthcare technologies by gender; Health Foundation[3].
3.2 Age
There is some evidence from studies that older age groups are more willing to trust health research and share data. For example, an NIHR[24] report showed that 80% of those aged 55+ thought health research had been very important in tackling COVID-19, dropping to 56% for ages 18-24. This is reflected in the Ipsos surveys on public attitudes towards science[25], conducted on behalf of UKRI during the first phase of the pandemic in 2020. 57% of those aged 16-25 thought science was more beneficial than harmful, compared to 66% of those aged 55-75 and 78% of those aged 76+.
The Health Foundation report[3], published in 2023, found that 57% of those aged 16-24 trusted NHS organisations with their data, rising to closer to 80% for those aged over 65.
Conversely, the NHS 2024 survey[6] identified the unfamiliar and unsure segment (Table 1) – those who have faith in the NHS, but feel less in control of their data – as primarily in the aged 65+ group. This is likely reflects the digital exclusion felt by some in that group referred to in section 2.3.
3.3 Geography
Whilst the NHS data saves lives survey[6] is focused on England only, similar surveys in Wales and
Scotland reflect the same trends. A 2023 public dialogue undertaken by Ipsos Scotland[26] and commissioned by the Scottish Government and Research Data Scotland looked at attitudes towards sharing citizen’s data within Scotland’s public sector. Whilst not a quantitative review, the participants still reflected similar trends to those reported in England, with people generally trusting the public sector’s use of data, but only when it had a clearly defined purpose
and scope, and clear public benefit.
A 2024 National Centre for Social Research public dialogue[27], commissioned by the Welsh Government, showed
that many of the participants were comfortable with sharing health data, provided the conditions discussed before, such as transparency and societal benefit, were met.
In comparison there is very limited data from Northern Ireland. The most recent and relevant report (Public attitudes towards data sharing in Northern Ireland[28]) is based on data from the 2015 Northern Ireland Life and Times Survey. Regardless, it still reflects the trends seen across the other nations, with a high proportion of respondents trusting their GP surgery (91%) and NHS (86%) to keep data secure and use it appropriately. These was slightly lower trust in academic researchers (72%) and much lower in commercial organisations (41%).
These trends are not just limited to the UK. A recent survey[29] in Denmark, a country where data reuse is considered fully incorporated into everyday life, also showed that most respondents were positive towards publicly funded researchers being allowed access to health data – up to 78% – with the proportion declining to 39% for access by commercial pharmaceutical companies.
In the US similar trends emerge. A 2024 paper[30] reviewing attitudes to the National Institute for Health’s data
policy showed that 95% would share data with their healthcare professional, declining to 73% for public health organisations and only 53% for private foundations. The same paper shows, however, that despite similar trends, trust in general is lower in the US. Significantly fewer people feel comfortable with sharing health data not only with their doctors, but also with their governments and research institutions than in the UK. The differences between the two health systems could be a factor, with the lower trust in the US potentially reflecting the privatised (and therefore more commercial) nature of its healthcare system, aligning with the general UK findings that people want to see clear societal benefits when sharing data.
3.4 Ethnicity
The data on how ethnicity affects public attitudes towards sharing health data is limited and mixed. In addition, while not the focus of this report, but still of relevance, the quality of the data collected on ethnicity is itself an issue. The Office for National Statistics compared the ethnicity health data recorded by the NHS in 2023 with the 2021 Census data and highlighted the highest level of agreement between the two sources for White British (95%), falling to 79% for Chinese and less than 7% for Gypsy or Irish Travellers[31].
This discrepancy, and the challenges of accurately collecting and using ethnicity data consistently, impacts the quality of the research based on health data. Some projects are addressing these challenges, such as Wellcome supporting a number of initiatives to improve categories and consistency[32].
An Understanding Patient Data report into attitudes towards using health data for planning[33] found that those from a minority ethnic background were more likely to know some or a lot about how the NHS uses patient data than those from white backgrounds (59% compared to 37%). It also reflects the finding from the HRA report[1], with slightly lower support for the use of patient data within the NHS from minority ethnic backgrounds, with 78% agreeing compared to 86% from white backgrounds.
The HRA report[1] into attitudes towards health research (considering it as a proxy for health data in this case) highlights that Black adults are less likely than white adults to trust or participate in government research, and more likely to take part in industry-funded studies:
- White adults are particularly averse to taking part in research funded by a private business – just under half say they are less likely to take part in a privately-funded study (47%).
- This is not the case for minority ethnic adults. Asian adults are twice as likely to say private-funded research encourages participation (18% Asian, 9% white adults) and this rises to over a third of Black adults (36%). On the other hand, finding out a study is funded by the government discourages Black adults (28% would be less likely to participate).
- Adults from a minority ethnicity are more likely than white adults to say research transparency in industry-funded studies makes them more confident in the findings (57% compared to 49%), but this is predominantly driven by Black adults (67%) who report this more than any other ethnic minority.
Black adults are also less confident that they would be treated with dignity and respect while taking part in research with 30% saying they are not confident compared to 20% of Asian adults and 18% of white adults[1].
In the context of broader systemic racial inequalities of the healthcare system and historical mistreatment of people from minority ethnic backgrounds, these results are unsurprising. Recent coverage of past experimentation on minority ethnic communities without consent, such as the radioactive chapatis given to Indian women in Coventry in the 1960s[34], demonstrates the extent of the issues and the challenges in rebuilding trust.
3.5 Digital access
As mentioned in section 2.3, the digital divide is relevant as digital access and confidence is a critical factor in how people feel about sharing healthcare data. The six segments identified by the 2024 NHS survey[6] were also given a measure of online confidence (Table 1). The three groups least likely to share health data – those unfamiliar and unsure, disengaged or sceptics – were also most likely to have low confidence online.
There are limitations to all these surveys in how accurately they represent those who are digitally excluded, given that most of the methodologies involve online surveys of some kind. However, we can draw some conclusions from more general surveys done on digital inclusion and health, such as the Ada Lovelace Institute’s report on the digital divide[35].
This 2021 report showed that, despite being conducted at the height of the pandemic, 60% of respondents had not heard of symptom trackers such as Zoe. Those who had heard of them or used them were much more comfortable with using them than those who did not. For symptom tracking apps over 90% of those who used it were ‘very’ or ‘quite’ comfortable with it compared to 66% who had not used it.
Other reports such as the Good Things Foundation’s Digital Nation[36] report collates information from various sources to provide a picture of digital access across the UK:
- 33% of those offline say it is difficult to interact with NHS services
- 25% of people with a disability or health condition, 48% of people with no formal qualifications and 37% of those aged over 65 lack basic digital skills
Given the numbers of people who are digitally excluded or unconfident online, and the correlation to their willingness to share health data, reaching this group could have significant impact. The Good Things Foundation is working towards hyperlocal interventions with its National Digital Inclusion Network, as well as projects such as Digital Communities Wales, the Scottish Council for Voluntary Organisations and Digital Unite’s digital champions.
3.6 Socio-economic and educational backgrounds
With socioeconomic status being strongly correlated to digital access[37], it is unsurprising that it follows similar patterns with respect to health data sharing.
The 2023 Health Foundation report[3] demonstrates significantly less support for healthcare technologies for those in the lowest socioeconomic group E compared to the highest, group A[38]. And the 2024 NHS survey[6] found a correlation between support for data sharing and socioeconomic group (Figure 4), with higher percentages of people in groups A and B (the two highest socioeconomic groups) in the confident and cautious data sharer segments. Interestingly, however, socioeconomic groups are evenly represented across the NHS and privacy sceptics segment (Table 1).
The survey also found that there are higher levels of degree education in the groups that are most likely to share data with the NHS (confident data enthusiasts, neutral followers and cautious data sharers). The groups least supporting of health data sharing – the disengaged and health data protective segment and the NHS and privacy sceptics segment – had the lowest levels of degree education, with around two-thirds in both segments having no degree, compared to just under half (46%) in confident data enthusiasts and even less (39%) in cautious data sharers. Over half (52%) of the cautious data sharers group have a degree level education[39].
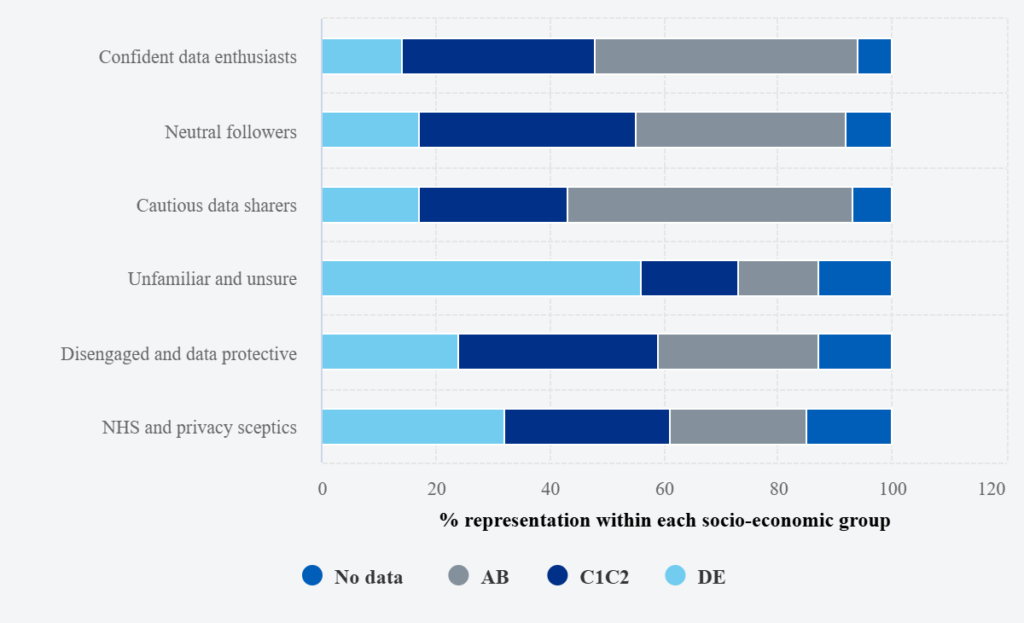
Fig 4: NHS segmented groups by socio-economic composition[41]. ABC1 are the three higher social and economic groups based on occupations, C2DE are the lower groups. These definitions are from the Market Research Society[42].
3.7 Patients with long-term health conditions (LTHCs)
There are some interesting studies into how having a LTHC affects attitudes towards sharing health data.
The Engineering and Physical Sciences Research Council (EPSRC)-funded project INTUIT[40] ran from 2018-2022 and looked at the sharing of health and lifestyle data for individuals with HIV. A research paper[41] from the project, published in 2022, looked at the barriers in sharing self-generated health data for those with LTHCs. 250 people with a range of conditions were surveyed, with 75% of respondents recording data daily, whether through written diaries or technology such as phones and smartwatches. Despite this, over two-thirds (67%) said they rarely or never share this data, even with their healthcare professionals, although very few (8%) are negative about sharing. Half of respondents were neutral towards the experience of sharing, with the rest (42%) being positive.
The NHS report[6] shows higher levels of people reporting a disability in the unfamiliar and unsure segment (48%), but with lower levels in the disengaged and data protective group (29%) (Table 1).
3.8 Health Care Professionals (HCPs)
HCPs and the general public share similar attitudes on how data is used. A 2022 Understanding Patient
Data report[42] looking at how primary care professionals in the UK view and use health data showed the highest agreement in sharing data is for patient care and care coordination in a local way such as across the practice or Primary Care Network, with 94% comfortable in sharing across their practice. This support reduces when shared across the wider NHS (51%), and significantly more when shared beyond the NHS, such as with a third-party organisation, where it drops to 17%.
There is a similar pattern with regards to sharing data for planning or research purposes, although somewhat running counter to this a higher percentage agreed they were comfortable in sharing data for research purposes outside the NHS (28%) than for care and coordination (18%).
The samples of HCPs are too small to draw any conclusions across devolved nations, although a review of global studies[43] has found similar trends with support for sharing between HCPs the highest (80%) followed by universities (62%) then pharmaceutical companies, governments and nonprofits (all around 40-45%), with the lowest being insurance companies at 27%.
3.9 Other demographics
There is little to no data analysis available on how attitudes vary by other protected characteristics, including religion,
sexual orientation, gender reassignment, and disability. Neither is there any information on how situations such
as being a carer impacts attitudes, aside from the NHS survey[6] reporting that the cautious data sharer segment contain a higher proportion of people with caring responsibilities (for children or people with disabilities), which may be due to the age profile of this group.
4. Get in touch
If you have any questions about the content of this document, or would like to share relevant research please get in touch at involvement@hdruk.ac.uk.
5. Acknowledgements
With thanks to Katie Weeks Consulting for conducting the literature review and bringing the content in this document together.
Thank you also to the following who provided comment:
- Aisha Kekere-Ekun (Public Partner, Health Data Research UK)
- Jack Palmer (Co-Production Officer, Health Data Research UK Wales)
- Cassie Smith (Director of Legal, Trust and Ethics, Health Data Research UK)
- Doreen Tembo (Head of Patient and Public Involvement and Engagement, Health Data Research UK)
- Ester Bellavia (Senior Patient and Public Involvement and Engagement Manager, Health Data Research UK)
- Clare Matysova (Programme Manager for Equity, Diversity and Inclusion, Health Data Research UK)
This report was commissioned by Anna Woolman (Public Engagement and Communications Manager, Health Data Research UK).
6. References
- https://www.hra.nhs.uk/planning-and-improving-research/best-practice/public-perceptions-research/
- https://www.nihr.ac.uk/news/nihr-survey-reveals-publics-attitudes-health-research-following-coronavirus
- https://www.health.org.uk/reports-and-analysis/briefings/exploring-public-attitudes-towards-the-use-of-digital-health
- https://zenodo.org/records/13353747
- https://www.involve.org.uk/sites/default/files/field/attachemnt/120727RCUKReview.pdf
- https://digital.nhs.uk/data-and-information/keeping-data-safe-and-benefitting-the-public/public-attitudes-to-data-in-the-nhs-and-social-care
- https://acmedsci.ac.uk/file-download/6616969
- https://wellcome.org/sites/default/files/public-attitudes-to-commercial-access-to-health-data-wellcome-mar16.pdf
- https://www.bbc.co.uk/news/health-26259101
- https://www.bbc.co.uk/news/technology-58761324
- https://www.theguardian.com/society/2021/aug/22/nhs-data-grab-on-hold-as-millions-opt-out
- https://www.hdruk.ac.uk/covid-19-data-and-connectivity/
- https://www.pioneerdatahub.co.uk/blogs/12-things-weve-learnt-about-covid-19-from-health-data-research/
- https://bmjopen.bmj.com/content/12/4/e057579
- https://www.theguardian.com/politics/2025/jan/13/labour-ai-action-plan-nhs-patient-data-why-causing-concern
- https://www.goodthingsfoundation.org/discover/digital-inclusion-insights/digital-inclusion-insights-2024/how-deep-is-the-uks-digital-divide
- https://journals.sagepub.com/doi/full/10.1177/20552076221089798
- https://zenodo.org/records/10894877
- A review of attitudes towards the reuse of health data among people in the European Union: The primacy of purpose and the common good – ScienceDirect
- https://doi.org/10.1093/fampra/cms036
- https://understandingpatientdata.org.uk/sites/default/files/201707/Identifiability%20briefing%205%20April.pdf
- https://digital.nhs.uk/data-and-information/keeping-data-safe-and-benefitting-the-public/public-attitudes-to-data-in-the-nhs-and-social-care/segmentation
- https://www.mrs.org.uk/resources/social-grade
- https://www.nihr.ac.uk/news/nihr-survey-reveals-publics-attitudes-health-research-following-coronavirus
- https://www.ipsos.com/sites/default/files/ct/news/documents/2020-09/20-031763-01_ukri_covid19_tracking_report_210920_public_0.pdf
- https://sciencewise.org.uk/wp-content/uploads/2024/08/public-dialogue-use-data-public-sector-scotland-findings-pilot-public-engagement-panel-scottish-government-report-commissioned-scottish-government.pdf
- https://healthandcareresearchwales.org/sites/default/files/202410/Public_Dialogue_Use_Data_Identifying_Approaching_Individuals_Research_Report.pdf
- https://www.ark.ac.uk/pdfs/Researchreports/Data_Sharing_Report.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11671018/
- https://pubmed.ncbi.nlm.nih.gov/39197051/
- https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthinequalities/articles/understandingconsistencyofethnicitydatarecordedinhealthrelatedadministrativedatasetsinengland2011to2021/november2023
- https://wellcome.org/news/ethnicity-categories-uk-health-data
- https://understandingpatientdata.org.uk/sites/default/files/202405/UPD_Data_for_Planning_Report_Final.pdf
- https://www.theguardian.com/news/2025/feb/11/the-coventry-experiment-why-were-indian-women-in-britain-given-radioactive-food-without-consent
- https://www.adalovelaceinstitute.org/wp-content/uploads/2021/03/The-data-divide_25March_final-1.pdf
- https://www.goodthingsfoundation.org/policy-and-research/research-and-evidence/research-2024/digital-nation.html
- https://www.thebritishacademy.ac.uk/documents/4427/Understanding_Digital_Poverty_and_Inequality_in_the_UK_full_report_2.pdf
- https://www.mrs.org.uk/resources/social-grade
- https://digital.nhs.uk/data-and-information/keeping-data-safe-and-benefitting-the-public/public-attitudes-to-data-in-the-nhs-and-social-care/segmentation
- https://intuitproject.org/
- https://journals.sagepub.com/doi/10.1177/20552076221084458
- https://understandingpatientdata.org.uk/primary-care-professionals-views-use-health-data
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10963197/#sec3
